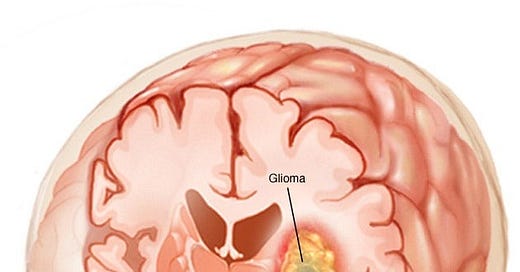
Glioma
A glioma is a tumor that forms in the brain or spinal cord. There are several types, including astrocytomas, ependymomas and oligodendrogliomas. Gliomas can affect children or adults. Some grow very q
What is a glioma?
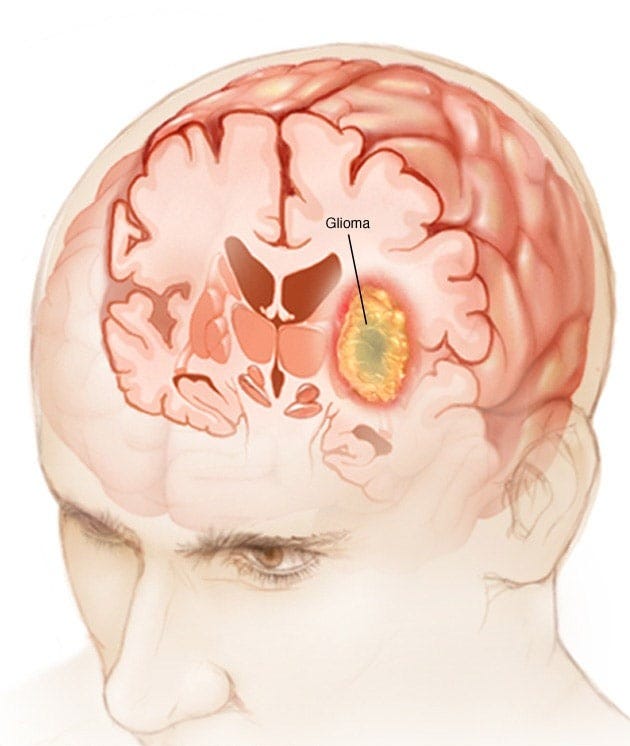
A glioma is a tumor that forms when glial cells grow out of control. Normally, these cells support nerves and help your central nervous system work. Gliomas usually grow in the brain, but can also form in the spinal cord.
Gliomas are malignant (cancerous), but some can be very slow-growing. They’re primary brain tumors, meaning they originate in the brain tissue. Gliomas don’t usually spread outside of the brain or spine, but are life-threatening because they can:
It is hard to reach and treat with surgery.
Grow into other areas of the brain.
Are there different types of gliomas?
There are three main types of gliomas, grouped by the type of glial cell they start in. Some gliomas contain multiple types of cells. Healthcare providers call these mixed gliomas. They categorize each type of glioma as low-, mid, or high-grade based on how fast they grow and other features.
Gliomas include:
Astrocytomas, including glioblastomas and diffuse intrinsic pontine gliomas (DIPGs):
Astrocytomas are a type of glioma that originates from astrocytes, star-shaped glial cells in the brain. Glioblastomas are a particularly aggressive type of astrocytoma, while diffuse intrinsic pontine gliomas (DIPGs) are a specific, highly aggressive form found in the brainstem of children.
Astrocytomas:
Definition: Astrocytomas are tumors that arise from astrocytes, a type of glial cell that supports and protects nerve cells in the brain.
Grading: Astrocytomas are graded based on their aggressiveness, with Grade I being the least aggressive and Grade IV (glioblastoma) being the most aggressive.
Location: While astrocytomas can occur in various parts of the brain, they are more common in the cerebrum of adults and the cerebellum in children.
Glioblastomas:
Definition: Glioblastoma (GBM) is a Grade IV astrocytoma, meaning it is the most malignant and aggressive type of astrocytoma.
Characteristics: Glioblastomas are characterized by rapid growth, necrosis (cell death), and the formation of abnormal blood vessels.
Prevalence: Glioblastomas are the most common malignant brain tumor in adults.
Diffuse Intrinsic Pontine Gliomas (DIPGs):
Definition:
DIPG is a specific type of astrocytoma that occurs in the pons, a part of the brainstem.
Characteristics:
DIPGs are highly aggressive, difficult to treat, and primarily affect children, with a peak onset between 6 and 9 years of age.
Prognosis:
DIPG carries a very poor prognosis, with a median survival of around 9 months after diagnosis and less than 10% of patients surviving beyond two years.
Location:
The pons, where DIPGs form, is crucial for controlling vital functions like breathing, heart rate, and eye movements, making treatment challenging.
Astrocytomas are a broad category of brain tumors, with glioblastomas being the most aggressive adult form and DIPGs being a particularly aggressive and devastating pediatric brainstem tumor.
Ependymomas:
Ependymoma is a type of brain and spinal cord tumor that originates from ependymal cells, which line the ventricles (fluid-filled spaces) of the brain and the central canal of the spinal cord. These tumors are relatively rare, accounting for about 2-3% of all primary brain tumors, and can occur in both children and adults.
Key Characteristics:
Origin:
Ependymal cells, which produce cerebrospinal fluid (CSF) and line the ventricles and central canal.
Location:
Most commonly found in the posterior fossa (around the fourth ventricle) in children, but can also occur in the supratentorial region (upper brain) or spinal cord.
Spread:
Ependymomas can spread through the CSF, potentially reaching other parts of the brain and spinal cord, but rarely spread outside the central nervous system.
Grading:
Ependymomas are graded based on their aggressiveness (how quickly they grow and spread), with grades ranging from 1 (low-grade, slow-growing) to 3 (high-grade, more aggressive).
Symptoms:
Symptoms vary depending on the tumor's location and can include headaches, nausea, vomiting, seizures, vision changes, balance problems, and neurological deficits.
Treatment and Prognosis:
Surgery:
Surgical removal of the tumor is the primary treatment to achieve a complete resection (removal of the entire tumor).
Radiation therapy:
Radiation therapy may be used after surgery, especially for incompletely resected tumors or in cases of higher-grade ependymomas.
Chemotherapy:
Chemotherapy is less commonly used but may be considered, particularly for recurrent or metastatic tumors.
Prognosis:
Prognosis varies depending on the tumor's grade, location, and extent of resection. Complete surgical removal offers the best chance of long-term survival.
Important Considerations:
Ependymomas are relatively rare, making them challenging to diagnose and treat.
The potential for CSF dissemination requires careful monitoring and follow-up.
Research continues to explore new treatment options, including targeted therapies and immunotherapies.
Oligodendrogliomas:
Oligodendrogliomas are a type of glioma, a brain tumor that originates in glial cells. Specifically, they arise from oligodendrocytes, which are cells that support and protect nerve fibers in the brain. These tumors are relatively rare and are most often found in adults, though they can occur in children as well.
Key Characteristics:
Origin:
Oligodendrocytes, the cells that form myelin sheaths in the central nervous system.
Location:
Commonly found in the frontal and temporal lobes of the brain.
Genetic Alterations:
Often associated with specific chromosomal deletions, particularly of the short arm of chromosome 1 and the long arm of chromosome 19 (1p19q codeletion).
Symptoms:
Seizures are a common initial symptom, and other potential symptoms include headaches, personality changes, weakness, and speech or memory problems.
Treatment:
Treatment options include surgery, radiation therapy, and chemotherapy, with the specific approach depending on the tumor's grade and location.
More Details:
Oligodendrogliomas are classified as a type of glioma, which are tumors that develop from glial cells, the supportive tissue of the brain. Oligodendrocytes are a type of glial cell that produces myelin, a fatty substance that insulates nerve fibers. The tumors are classified as either grade 2 (low-grade) or grade 3 (anaplastic), with grade 3 oligodendrogliomas being more aggressive.
Symptoms:
The symptoms of oligodendrogliomas can vary depending on the tumor's location and size. Seizures are a frequent initial symptom, and other potential symptoms include headaches, changes in mood or personality, weakness or numbness on one side of the body, speech difficulties, and memory problems.
Diagnosis and Treatment:
Diagnosis typically involves imaging scans like MRI, along with biopsy and genetic testing to confirm the presence of a tumor and its specific characteristics. Treatment often involves surgical removal of the tumor, followed by radiation therapy and/or chemotherapy, particularly for grade 3 tumors or when the tumor cannot be completely removed surgically.
Who is at risk of getting a glioma?
Anyone can develop a glioma, but the following factors may increase your risk:
Age: Gliomas are most common in older adults (over 65) and children (under 12).
Ethnicity: White people may be more likely to develop gliomas than other races.
Family history: Some inherited genetic disorders may increase your risk of gliomas.
Sex: Gliomas are slightly more common in men than women.
Radiation or toxin exposure: Repeated or prolonged exposure to radiation or certain chemicals may increase your risk.
How common are gliomas?
About 80,000 people are newly diagnosed with primary brain tumors each year in the U.S. Approximately 25% of these are gliomas.
Symptoms and Causes
What causes gliomas?
Research suggests that changes to DNA lead to the development of brain tumors and spinal cord tumors like gliomas. Our genes contain DNA. They give instructions to cells about how to grow and multiply. Mutations, or changes, to the DNA in our genes, can cause cells to multiply out of control.
It’s possible to inherit genetic mutations from your parents. They can also occur suddenly during your lifetime.
What are the symptoms of gliomas?
Symptoms of gliomas may include:
Aphasia (problems with speaking and communicating).
Changes in your vision or vision loss.
Cognitive problems (trouble thinking, learning, or remembering).
Difficulty walking or keeping your balance.
Dizziness.
Headaches.
Hemiparesis (weakness or numbness on one side of the body).
Nausea and vomiting.
Personality or behavioral changes.
Seizures.
What are the complications of gliomas?
Potentially life-threatening complications of gliomas include:
Brain hemorrhage (bleeding in the brain).
Brain herniation (brain tissue moves outside its normal position in the skull).
Hydrocephalus (fluid buildup in the brain).
The pressure inside your skull.
Seizures.
Diagnosis and Tests
How are gliomas diagnosed?
Your healthcare provider evaluates your symptoms and reviews your medical history. They’ll also do a complete physical and neurological exam.
MRIs and CT scans are the most common imaging scans for brain tumors. Your healthcare provider looks for tumors in your brain, as well as tumors elsewhere in your body.
If your healthcare provider sees an abnormal mass on your imaging scans, they’ll do a biopsy. A biopsy is a procedure to analyze a sample of tissue. The biopsy will help them determine:
If the tumor is cancerous.
If the tumor is the result of an abnormal gene.
The type of cells in the tumor.
The grade (aggressiveness) of the tumor.
Management and Treatment
How is a glioma treated?
Your treatment plan for a glioma depends on several factors, including:
If you’ve had brain cancer treatment in the past.
The location, type, and size of the tumor.
Your age.
Your health.
For most people, surgery is the first treatment for a glioma. A surgeon may be able to remove all of the tumor they can see if it’s easily accessible. But gliomas can be hard to remove completely, especially hard to reach or near delicate areas of the brain.
Additional treatments, such as chemotherapy and radiation therapy, should follow surgery. These are adjuvant therapies, meaning they destroy any remaining cancer cells or parts of the tumor after surgery. But if a tumor is inoperable, your provider might use chemotherapy or radiation therapy as your primary treatment.
Surgery
A craniotomy (open brain surgery) is the most common type of surgery to remove gliomas. Depending on the size and location of the tumor, you may be a candidate for laser ablation. This minimally invasive surgery uses heat from a laser to destroy all or part of a brain tumor.
A surgeon may use special techniques, such as imaging or brain mapping, to guide the surgery. Brain mapping shows which areas of your brain control vital functions. This information helps your surgeon avoid removing or harming healthy brain tissue.
Radiation
Radiation therapy uses powerful doses of radiation to destroy tumors. Your healthcare provider may recommend radiation therapy for gliomas. Radiation therapy targets the exact shape of the tumor, minimizing the risk of damage to surrounding tissues.
You may also receive a form of radiation therapy called brachytherapy. A healthcare provider applies radiation sources close to the tumor to treat it. The sources release radiation without harming nearby tissues.
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells. It treats many types of cancer. This treatment may be oral or intravenous.
Temozolomide is a common chemotherapy medicine that is given to improve the efficacy of radiation therapy.
Outlook / Prognosis
What is the outlook for people with gliomas?
Survival rates for gliomas vary by tumor type, tumor grade, and a person’s age. Certain mutations can also affect the prognosis. The older someone is when they’re diagnosed and treated, the worse the outlook. The five-year survival rate for adults and children is highest for low-grade ependymomas, oligodendrogliomas, and astrocytomas. The lowest (between 6% and 20%) for glioblastomas.
Prevention
How can I prevent gliomas?
Most risk factors for gliomas, such as age and race, aren’t controllable. However, early detection and treatment of low-grade gliomas may slow or prevent their progression into high-grade gliomas. If brain tumors run in your family, you may want to consider genetic testing. Talk to your healthcare provider or a genetic counselor about the risks and benefits of genetic testing.
It is also a good idea to:
Limit radiation exposure to your head.
Maintaining a healthy lifestyle.
Living With
What should I do if I have a glioma?
After treatment, stay in close communication with your healthcare provider. You’ll need regular imaging scans to see if the cancer returns.
Brain cancer treatment can cause damage to healthy brain tissue. Rehabilitation with physical therapists or occupational therapists can help you regain skills like walking, speaking, and remembering.
Support groups for you and your family can help you manage the physical and emotional challenges of living with a brain tumor.
What should I ask my healthcare provider?
If you have a glioma, you may want to ask your provider the following questions:
What is the cancer’s type and grade?
What treatments are right for me?
Will treatment affect my cognitive function?
Are there clinical trials I can take part in?
Can the cancer come back after treatment?