Inflammatory Bowel Disease (IBD) & Cancer Risk!
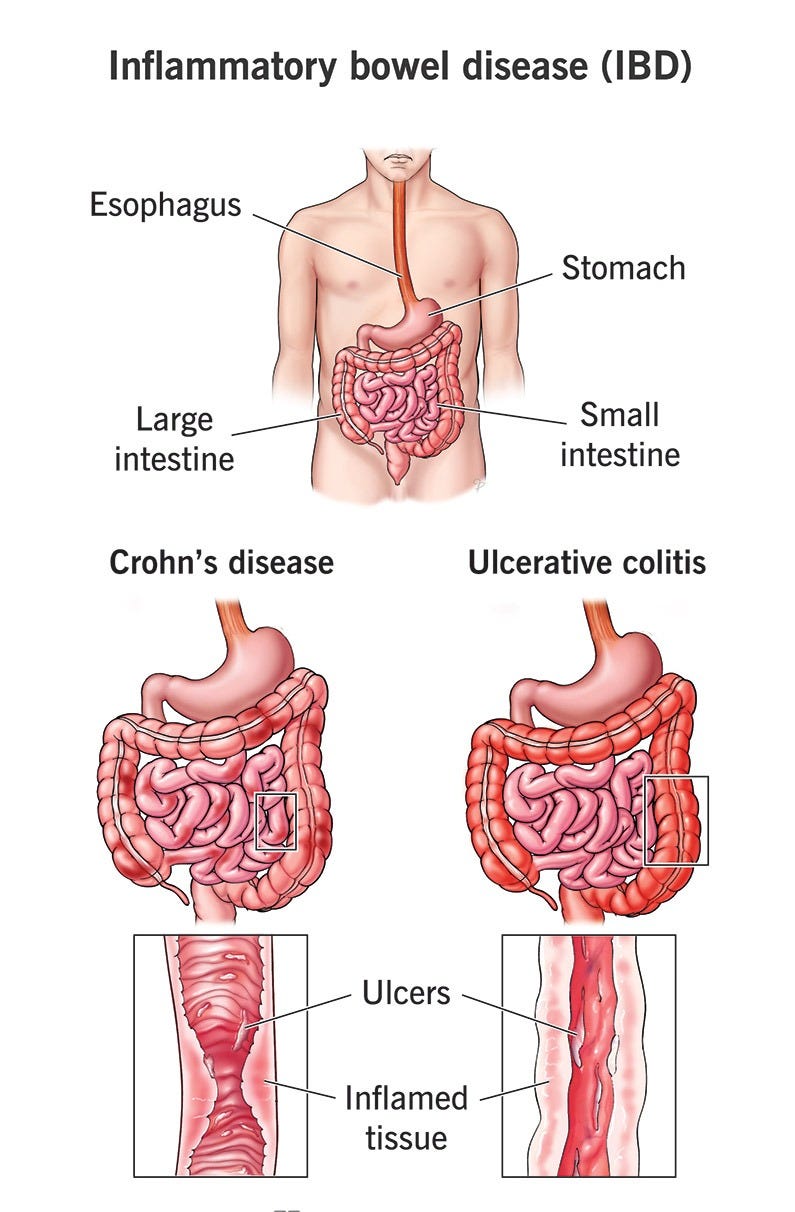
Inflammatory bowel disease (IBD) includes Crohn’s disease and ulcerative colitis. IBD causes symptoms like belly pain and cramps, diarrhea and blood in your poop (stool). Inflammatory bowel disease is
What is inflammatory bowel disease (IBD)?
Inflammatory bowel disease (IBD) refers to a group of diseases that cause chronic inflammation in the gastrointestinal (GI) tract. Its symptoms may come on suddenly (flares) and cause intense stomach cramps and diarrhea, among other issues. But IBD can affect more than your gut — it can affect your overall physical health, emotional well-being, and even your mental health.
Inflammatory bowel disease is a lifelong illness for which there’s no cure. This may sound grim. But some treatments manage IBD symptoms, and steps you can take to keep IBD from disrupting your life.
Types of IBD
Crohn’s disease and ulcerative colitis are the main types of IBD:
Crohn’s disease: Crohn's disease is a type of inflammatory bowel disease (IBD) that causes swelling and irritation of the tissues, called inflammation, in the digestive tract. This can lead to belly pain, severe diarrhea, fatigue, weight loss, and malnutrition.
Inflammation caused by Crohn's disease can affect different areas of the digestive tract in different people. Crohn's most commonly affects the end of the small intestine and the beginning of the large intestine. The inflammation often spreads into the deeper layers of the bowel.
Crohn's disease can be both painful and debilitating. Sometimes, it may lead to serious or life-threatening complications.
There's no known cure for Crohn's disease, but therapies can greatly reduce its symptoms and even bring about long-term remission and healing of inflammation. With treatment, many people with Crohn's disease can function well.
Ulcerative colitis (UC): Ulcerative colitis is a type of inflammatory bowel disease (IBD) that causes inflammation and sores, called ulcers, in part of the digestive tract. Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) affects the innermost lining of the large intestine, called the colon, and rectum. Symptoms usually develop over time, rather than coming on suddenly.
Ulcerative colitis can weaken the body and can sometimes lead to life-threatening complications. While it has no known cure, treatment can greatly reduce and relieve symptoms of the disease. It also may bring about long-term remission.
How common is IBD?
Inflammatory bowel disease (IBD) is quite common, affecting a significant number of people globally. In the United States, it's estimated that 1.6 million people are living with IBD. The Crohn's & Colitis Foundation reports that as many as 70,000 new cases are diagnosed each year, and there may be as many as 80,000 children in the US with the condition. In Canada, Crohn's and Colitis Canada estimates that 322,600 people were living with IBD in 2023, and this number is projected to rise to 470,000 by 2035. Globally, it's estimated that over 10 million people have IBD.
Symptoms and Causes
What are the symptoms of inflammatory bowel disease?
IBD symptoms may be mild or severe. They come and go, and you can’t always predict when they’ll happen. When they do, a healthcare provider may say you’re having an IBD flare (active disease). When your symptoms go away after treatment, a provider may say the disease is in remission. Common IBD symptoms include:
Lower abdominal pain that may feel like stomach cramps.
Blood in your poop (stool).
Chronic diarrhea.
Fatigue.
Unintended weight loss.
Conditions commonly mistaken for IBD
Some conditions are commonly mistaken for inflammatory bowel disease (IBD) because they share some of the same symptoms. However, they are entirely different conditions, with different causes and treatments.
These include:
Irritable bowel syndrome (IBS).
Celiac disease.
IBD is not the same as irritable bowel syndrome (IBS)
Irritable bowel syndrome (IBS) causes uncomfortable or painful problems in your stomach. It is possible to have both IBS and IBD at the same time.
Similarities between IBS and IBD:
Both are life-long (chronic) conditions affecting the gastrointestinal (GI) tract.
Both can hurt a person's quality of life.
They share some symptoms, including stomach pain and changes in bowel movement.
Differences between IBS and IBD:
IBS does not cause inflammation (the most critical distinction).
IBS does not cause symptoms in other parts of the body (beyond the GI tract).
IBD is a kind of autoimmune disease, whereas IBS is not.
IBD causes physical damage to the digestive tract, whereas IBS does not.
IBD is not the same as celiac disease
Celiac disease is similar to IBD in some ways, and it is possible to have both at the same time.
Similarities between celiac disease and IBD:
Both are life-long (chronic) conditions related to the immune system.
Both can cause long-lasting problems.
Both can keep your body from getting all the nutrients it needs.
Differences between celiac disease and IBD:
Celiac disease is triggered by foods that contain gluten. Whereas IBD is thought to be triggered by complex interactions between genetics and the environment.
Celiac disease causes damage to the lining of the small intestine. However, different types of IBD can damage the entire digestive system and are not always confined to the intestinal lining.
What causes inflammatory bowel disease?
IBD happens when immune system cells in your GI tract mistakenly attack healthy tissue, causing inflammation that leads to Crohn’s disease and ulcerative colitis. Researchers don’t know the exact reason why this happens. But they’re studying mutations in certain genes that normally:
Keep your immune system on an even keel so it doesn’t overreact when it detects intruders.
Affect your mucosal barrier, which is the first line of defense in your intestine.
Control bacterial growth in your intestine.
When these genes mutate (change), it increases your risk of IBD. Researchers may call these genes susceptibility genes. There are more than 160 different susceptibility genes. If you inherited any number of them, several everyday activities could trigger IBD symptoms. These activities don’t cause the disease. Common IBD triggers include:
Antibiotics.
NSAIDS (nonsteroidal anti-inflammatory drugs).
Smoking cigarettes.
Stress.
Researchers are also investigating whether issues with your gut microbiome may play a part in the chronic inflammation that causes IBD.
Can food cause IBD symptoms?
No, but you may notice that your symptoms are worse after eat certain foods or liquids. Everyone is different, but food and drink that may make you feel worse may include:
Beverages with alcohol.
Caffeinated drinks.
Carbonated drinks.
Food made with milk.
Food with lots of fiber.
Greasy food.
What are the risk factors for IBD?
The most significant risk is having a family history of IBD. Studies show that 5% to 20% of people with IBD have a close family member — parent, sibling, or child — who has IBD.
What are the complications of inflammatory bowel disease?
IBD may cause other medical conditions in your GI tract and beyond. Some may be medical emergencies or serious illnesses, including:
Colon cancer: Having IBD increases the chance you’ll develop colon cancer.
Perforated bowel: Symptoms include severe belly pain and cramping, bloated belly, and pain when you touch your belly.
Toxic megacolon: Symptoms include bloody diarrhea, severe belly pain, and pain when you touch your belly.
Other IBD complications that affect your GI tract are anal fistula and anal stenosis. Anal stenosis is when your anal canal narrows, making it hard for poop to leave your body.
IBD may increase your risk of complications like:
Anemia (low levels of red blood cells).
Blood clots.
Eye pain and irritation.
Kidney stones.
Mouth sores.
Liver diseases like cirrhosis and primary sclerosing cholangitis.
Malabsorption and malnutrition.
Swollen joints.
Skin sores and rashes.
Weakened bones (osteoporosis).
Diagnosis and Tests
How do healthcare providers diagnose inflammatory bowel disease?
A healthcare provider will do a physical examination. They’ll ask about your symptoms, including how long you’ve had them, if your symptoms are mild or severe, and if they come and go. They may order the following tests:
Complete blood count (CBC).
Capsule endoscopy.
Colonoscopy.
Computed tomography (CT) scan.
EUS (endoscopic ultrasound).
Flexible sigmoidoscopy.
Magnetic resonance imaging (MRI) scan.
Upper endoscopy.
Management and Treatment
How is inflammatory bowel disease treated?
Treatments vary depending on the type of IBD that you have, but all treatments focus on bringing IBD into remission and keeping it there. A healthcare provider may prescribe medication to ease symptoms. In some cases, you may need surgery if medications aren’t effective.
Medication
In general, medications for IBD focus on managing inflammation and controlling your immune system’s response. Healthcare providers may use the same types of prescription medication to treat Crohn’s disease and ulcerative colitis. Medications may include:
Antibiotics: You may receive antibiotics if you have an infection from an anal fistula.
Antidiarrhea medication: If you have Crohn’s disease, your provider may prescribe medications like loperamide (Imodium® A-D).
Biologics: These medications calm your immune system, so it doesn’t release antibodies that trigger inflammatory bowel disease.
Corticosteroids: You may receive this medication for inflammation.
Immunomodulators and immunosuppressants: These medications also help to calm your immune system.
Surgery
IBD medication may manage your symptoms for many years. But if medications stop working, your provider may recommend surgeries like a colectomy.
Outlook / Prognosis
What can I expect if I have inflammatory bowel disease?
IBD is a chronic condition that you’ll need to manage for the rest of your life. Having this condition also increases your risk of serious illnesses like colon cancer.
For those reasons, you should plan on regular visits to your healthcare provider even when you don’t have symptoms. Your provider may recommend that you schedule appointments every six months when IBD is in remission, and more often when you have an IBD flare. If you’re in your 30s or 40s, your provider may recommend you start receiving routine colonoscopies earlier than most people.
Living With
How do I take care of myself?
It’s not always easy to live with IBD. Symptoms may flare up and then go away for weeks and months. You may find yourself wondering when the next flare will hit. You may feel embarrassed or self-conscious about symptoms like sudden bouts of diarrhea that make you race for the bathroom. Here are some suggestions that may help you manage IBD:
Eat well: Take time to track and identify foods and drinks that trigger your IBD. Talk to a dietitian about meal plans that avoid trigger foods and drinks but provide enough nutrition.
Track your symptoms during a flare: If you can pinpoint when you’re more likely to have symptoms, you can plan your day. That includes identifying restrooms so you know where to go when you need to go.
Pack an emergency kit: Accidents can and will happen. Consider carrying an emergency kit with spare underwear, panty liners, toilet tissue, and baby wipes. You may never need your ki,t but having it at hand may make you feel less anxious should you need it.
Share your situation: You may want to keep details about your IBD issue to yourself. That’s completely understandable. But consider telling a close friend or work friend about your IBD issues. It may help to have someone you can call on when you need help.
Manage your stress: Stress can trigger IBD symptoms. Stress management programs may reduce or delay your symptoms.
Seek support: Millions of people in the U.S. have IBD. There are support groups where you can spend time with people who know what you’re going through.
Consider mental health support: IBD may lead to depression. Talking to a psychologist may help.
Quit smoking: Research shows smoking cigarettes can trigger inflammatory bowel disease symptoms.
When should I see my healthcare provider?
Medication and self-care often help keep IBS in remission. But you should contact your healthcare provider if you have IBS flares that don’t go away.
When should I go to the emergency room?
If you have IBD, you have an increased risk of conditions like toxic megacolon or perforated bowel, which are medical emergencies. Call 911 (or your local emergency service number) or go to the emergency room if you have the following symptoms:
Fever above 100.3 degrees Fahrenheit (37.9 degrees Celsius) and chills could be signs of infection.
Severe abdominal cramping or pain that doesn’t go away.
Severe nausea and vomiting.
Rectal bleeding with clots of blood in your poop.
Swollen abdomen.
Additional Common Questions
What’s the difference between IBD and IBS?
Both IBD and IBS affect your gut. The difference is that IBD involves inflammation, but IBS doesn’t.
Here’s Why Ulcerative Colitis and Crohn’s Disease Increase Your Risk of Colon Cancer
Chronic inflammation from flare-ups can damage the lining of your intestinal wall, making your colon more vulnerable to cancer
Living with an inflammatory bowel disease (IBD) can mean facing a new normal. Nutritional plans, lifestyle changes and being physically active regularly can make a world of difference when you’re dealing with flare-ups from ulcerative colitis or Crohn’s disease.
But when these conditions go unnoticed, unmanaged or untreated for long periods of time, they can wreak havoc on your bowels and leave your intestines vulnerable to bigger problems like cancer.
Colorectal surgeon Scott Steele, MD, MBA, explains just how these chronic conditions are linked with colon cancer and what you can do to reduce your risk.
The link between ulcerative colitis, Crohn’s disease and cancer
Healthcare providers aren’t entirely sure what causes inflammatory bowel diseases like ulcerative colitis and Crohn’s disease. But they do know that they’re related to a dysfunctional immune response that occurs within your digestive tract.
When you have one of these chronic conditions, you can experience inflammation that builds up and spreads throughout your digestive tract — from your anus through your colon and all the way up to your stomach and small intestine (for Crohn’s).
With each flare-up, inflammation may worsen over time so that it causes damage to the lining of your intestinal walls, leaving them swollen, irritated and often covered in lesions or scar tissue. In an attempt to heal from these attacks, your cells try to recover and regrow. But this can lead to an over-abundance of cell growth resulting in polyps, precancerous growth and colorectal (colon) cancer.
“Anything associated with chronic inflammation is a risk factor for the development of colorectal cancer because chronic inflammation leads to a higher turnover of the lining of the cells in the colon, which may ultimately lead to the development of colorectal cancer,” explains Dr. Steele.
Of those with IBD, who is most at risk?
Some studies have found that people who have IBD are six times more likely to develop colorectal cancer than the general population. Recent studies show that IBD-related colorectal cancers have declined in recent decades due to improved cancer screenings and improved inflammation management. But several of the following factors have been identified to increase your risk for colon cancer if you’re living with IBD:
Being diagnosed with IBD at a young age.
Having inflammation on just the left side of your colon.
Having inflammation that affects most of your colon.
Having chronic inflammation for more than eight years.
Being immunocompromised or having a weakened immune system.
Genetic or hereditary conditions, like familial adenomatous polyposis (FAP) or Lynch syndrome.
Family history of IBD or colon cancer.
Primary sclerosing cholangitis (PSC), or chronic inflammation in your bile ducts.
“Certain disease processes go together, and ulcerative colitis and PSC in some patients are connected,” notes Dr. Steele. “When you have PSC, you tend to have more potent or worse colon inflammation and symptoms, which leads to a slightly higher risk of having colon cancer.”
Why colon cancer screening is important
“People who have been diagnosed with ulcerative colitis and Crohn’s disease should be getting exams regularly just to monitor their underlying disease, so they’re probably getting evaluated for colon cancer to begin with,” clarifies Dr. Steele.
“Certainly, if they have biopsies that show dysplasia, or abnormal tissues, we will follow those patients more often up to and including annually or every other year, depending on what the biopsies show.”
That means even if your IBD is in remission, you should still get screened for colon cancer regularly, especially if you haven’t been examined in the last five to 10 years. These screenings can help doctors catch colon cancer even in its precancerous and earliest stages of growth — and, during the examination, they can remove these areas of concern in real time.
“The unique thing about endoscopies is that they can detect tumors when someone is asymptomatic and they’re just at their infancy, at the dysplasia or small polyp stage,” states Dr. Steele.
“Other cancers, like pancreatic cancer, are oftentimes diagnosed at a later stage. But an endoscopy has the ability to detect polyps, early-stage lesions and multiple polyps throughout the colon, or to even give people a peace-of-mind that they don’t have anything growing in their colon.”
How to reduce your cancer risk
If you’re living with IBD, reducing your risk for cancer is directly tied to reducing IBD flare-ups. By focusing on healthy habits and lifestyle changes, you can help lower your risk for cancer by trying the following:
Avoid foods that trigger your inflammation.
Embrace a healthy nutritional plan that meets your dietary needs.
Avoid smoking and alcohol, which can worsen inflammation.
Stay physically active for 30 minutes a day most days a week.
Have routine cancer screenings and evaluations with your healthcare provider.
“Certainly, the development of cancer has multiple factors linked to it,” says Dr. Steele. “But it’s important that a healthy lifestyle includes regular screening examinations, and open communication with your healthcare provider is critical. Endoscopy has a role in colon screening and can even save your life.”